Eczema is a type of skin condition that is characterized by patches of red, cracked, rough, itchy, and inflamed skin. In some cases, blisters may also occur. People usually use the term ‘eczema’ to talk specifically about the most common form of eczema, i.e. atopic dermatitis. But there are other forms of eczema also, with their own triggers and symptoms.
The condition is not contagious and some foods such as dairy and nuts and certain environmental factors such as pollen and smoke may trigger its symptoms.
Demographics of eczema
Generally, eczema can happen to anyone and at any time of his/her life. Health statistics have shown that eczema is most prevalent during early childhood, usually affecting infants below 2 years old. According to the Australasian Society of Clinical Immunology and Allergy (ASCIA), there are three classifications of eczema, depending on the age of the person when eczema strikes:
- Infantile eczema
Most common during the first 6 months of life, and generally improves when the child reaches the age between 2 to 5 years old. Typical symptoms include a rash that is red and itchy, along with dry skin. - Childhood eczema
This may develop from infantile eczema or suddenly appear between the age of 2 to 4 years old, and usually improves with age. Although some children eventually outgrow this, most will continue into adulthood with a high tendency to develop dry and sensitive skin. Childhood eczema can affect the skin in elbow creases, behind the knees, and across the ankles. Sometimes skin on the face, neck and ears can get affected, too. - Adult eczema
Similar to childhood eczema, adult eczema generally affects skin at the neck, elbow creases, wrists, behind the knees and ankles; and affected areas usually appear very dry, red and itchy. Weeping may also appear in the area(s) affected by eczema. This condition generally has a tendency to improve in middle life; and although rare to appear in the elderly, there is still a chance that adult eczema appearing in the elderly.
General symptom of eczema
Eczema happens when your skin barrier is unable to repair itself, and has a decreased ability to retain water (moisture). This results in a loss of moisture, resulting in dry and scaly skin. With a poor healing ability, the skin exposes itself to environmental allergens and irritants. These enter the body and trigger an immune system response, i.e. inflammation. This is when skin becomes red, inflamed and itchy.
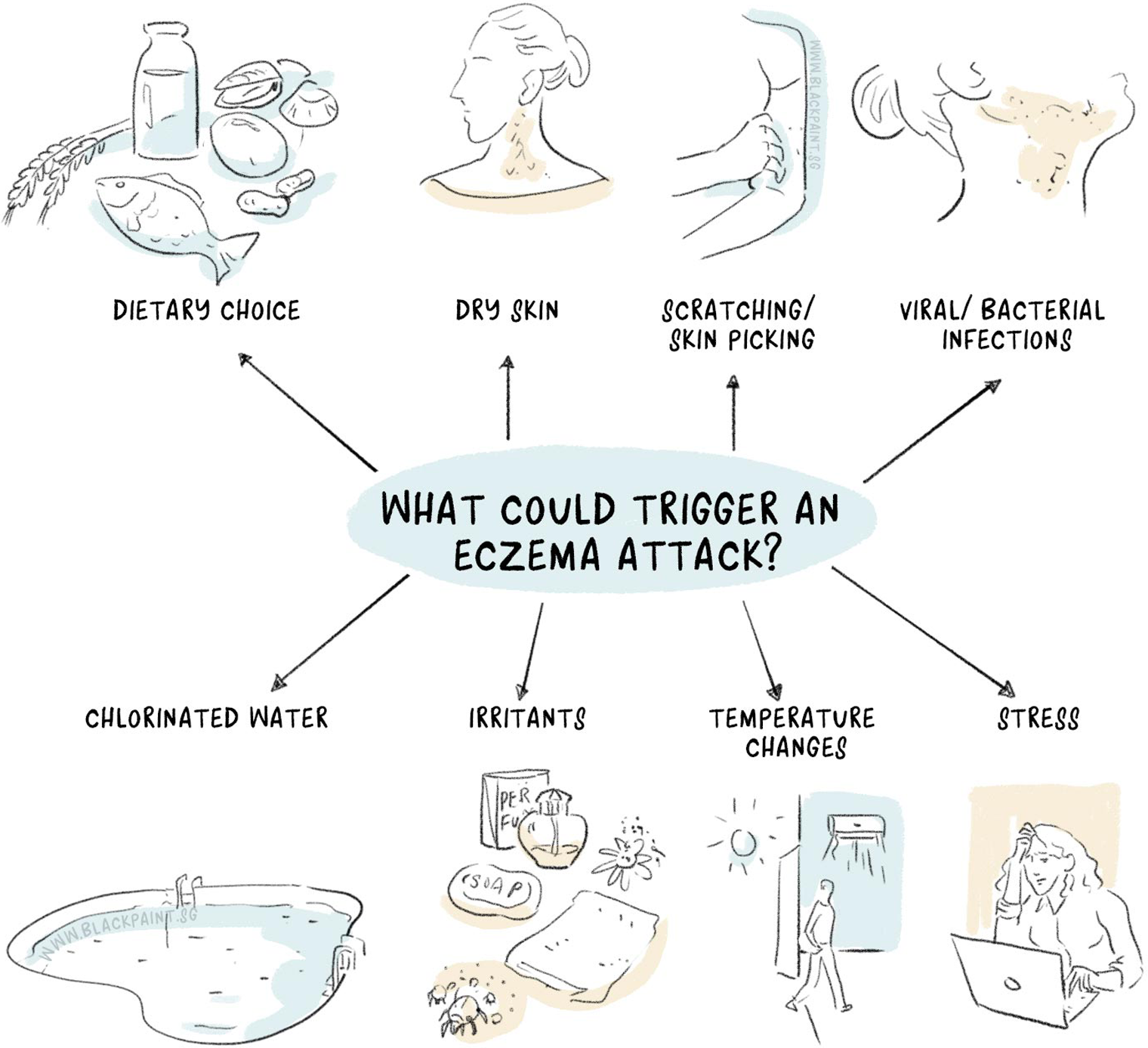
One is usually more inclined to get eczema if there is a family history of eczema or other allergic conditions, such as hay fever (allergic rhinitis) or asthma. Besides carrying a hereditary risk, environmental triggers and/or food allergies can also cause an eczema flare. An eczema flare happens when eczema worsens.
Types of eczema
The following are the different types of eczema:
1. Atopic dermatitis
The most common type of eczema, atopic dermatitis generally begins during childhood and may get milder or go away completely by adulthood. Atopic dermatitis forms a part of the atopic triad. The meaning of “Triad” is three. Apart from atopic dermatitis, the other diseases in this triad are hay fever and asthma. Many individuals who suffer from atopic dermatitis may also have all three conditions. This condition makes the skin itchy and red.
This is a chronic condition and you can have periods of flares of the disease with periods of complete remission in between.
Symptoms of atopic dermatitis
The symptoms of atopic dermatitis vary widely in different individuals and include:
- Dryness of skin
- Itching of the skin that can be severe particularly at night
- Formation of patches on certain areas of the skin that may be red or brownish-gray in color particularly on the hands, ankles, feet, neck, upper chest, wrists, on the inner side (bends) of the knees and elbows, eyelids, and in infants on the scalp and the face
- Formation of small, elevated bumps from which fluid may leak and may form a crust when you scratch them
- Cracked, scaly, and thickened skin
- Raw, swollen, and sensitive skin due to scratching
- Infection of the skin due to scratching

Causes of atopic dermatitis
Healthy skin in a person helps in retaining moisture and protecting them from irritants, bacteria, and allergens. Atopic dermatitis occurs when the natural barrier of your skin weakens implying that it is not fully capable of protecting you from irritants. The likely cause of atopic dermatitis is a combination of the following factors:
- Dry skin
- Genetic variation
- A problem in your immune system
- Irritants such as soaps, detergents, disinfectants, shampoos, juices from meats, vegetables or fresh fruits
- Allergens such as pets, dust mites, pollen, dandruff or mold
- Microbes such as viruses, certain fungi, and bacteria (Staphylococcus aureus)
- Very cold or hot weather, low and high humidity, and sweating during exercise may trigger your symptoms
- Foods such as eggs, dairy products, seeds and nuts, wheat, and soy products can cause flare-ups of atopic dermatitis (refer to section for solution specifically for “food allergy-related eczema”)
- Stress can worsen the symptoms of atopic dermatitis
- Women may experience increased symptoms of atopic dermatitis when there is a change in the hormone levels in their body such as at some times during their menstrual cycle, and during pregnancy
Risk factor of atopic dermatitis
The major risk factors that increase your likelihood of developing atopic dermatitis are having a family or personal history of allergies, eczema, asthma or hay fever.
2. Contact dermatitis
Contact dermatitis is characterized by an itchy, red rash that occurs as a result of an allergic reaction to a substance or when you touch it directly. The rash due to contact dermatitis isn’t life-threatening or contagious, but it is usually very uncomfortable. It is of two types: Irritant contact dermatitis occurs when an irritant such a chemical irritates the skin. Allergic contact dermatitis occurs when your immune system reacts to some irritant such as metal or latex.
Symptoms of contact dermatitis
The symptoms of contact dermatitis are the same as of atopic dermatitis but they appear on areas of the body, which are exposed directly to the irritating substance- for instance, beneath a watch band or along your calf, which came in contact with poison ivy. The rash generally develops within a few minutes or hours of getting in contact with the irritant and may last between two and four weeks.
Causes of contact dermatitis
Irritant contact dermatitis, the common of the two is a non-allergic reaction of the skin that occurs when an irritant damages the outer layer of your skin. Some of the common irritants that can cause irritant contact dermatitis are:
- Solvents
- Detergents and bleach
- Rubbing alcohol
- Solutions that you may use to produce permanent waves in hair, shampoos
- Plants
- Airborne substances including wool dust or sawdust
- Pesticides and fertilizers
Allergic contact dermatitis happens when an allergen (any substance that you may be sensitive to) triggers a reaction of the immune system (immune reaction) in the skin. The reaction usually occurs in the area of the skin that comes into contact with an allergen. However, the reaction may also occur by any substance that enters the body by way of flavorings, foods, medicine, or dental or medical procedures (also known as systemic contact dermatitis).
Some of the common allergens that can cause allergic contact dermatitis are:
- Nickel that is used to make buckles, jewelry, and other items
- Balsam of Peru that is present in several products such as cosmetics, perfumes, flavorings, and mouth rinses
- Medicines such as oral histamines and antibiotic creams
- Formaldehyde that is present in disinfectants, clothing, and preservatives
- Products of personal care such as body washes, deodorants, cosmetics, nail polish, and hair dyes
- Plants including mango and poison ivy in which a very allergenic substance referred to as urushiol is present
- Airborne substances including spray insecticides and ragweed pollen
- Products that can cause a reaction due to sun exposure (referred to as photoallergic contact dermatitis), including certain oral medicines and sunscreens
Children can develop contact dermatitis either from the allergens mentioned above or from getting in contact to diapers, sunscreens, baby wipes, and clothing containing dyes or snaps.
Risk factors of contact dermatitis
Some hobbies and jobs make you more prone to develop contact dermatitis. These include:
- Dental and health care employees
- Construction workers
- Metalworkers
- Cosmetologists and hairdressers
- Cleaners
- Auto mechanics
- Swimmers or scuba divers, because of the presence of rubber in goggles or face masks
- Agricultural workers and gardeners
- Cooks or other people who handle food
3. Dyshidrotic eczema
Dyshidrotic eczema or dyshidrosis is a type of eczema that is characterized by the formation of small blisters filled with fluid on the palms of hands, sides of fingers, and soles of feet. The blisters usually last for about three weeks at a time. They can lead to intense itching and once these blisters dry; the skin may look scaly. Furthermore, the blisters generally recur and in some cases they recur even before the healing of the previously present blisters occur.
Symptoms of Dyshidrotic eczema
Dyshidrotic eczema is characterized by the formation of blisters filled with fluid on the fingers, palms (of hands), soles (of feet), and toes. The blisters are generally small (the size of the lead of a pencil) and present in clusters. In severe cases, these blisters can merge and form large blisters. The area affected by dyshidrotic eczema may be very itchy and painful. Once these blisters flake off and become dry, which happens in around three weeks, the skin beneath them may become tender and red. The condition has a tendency to recur regularly for several months to years.

Causes of dyshidrotic eczema
What exactly causes dyshidrotic eczema remains unknown. It may occur in people who have atopic dermatitis and hay fever. Blisters may also erupt seasonally in people who have nasal allergies. Some of the common causes of dyshidrotic eczema are:
- The dampness of feet and hands
- Allergies
- Stress
- Exposure to certain substances including cobalt, chromium or nickel salt
Risk factors of dyshidrotic eczema
The risk factors of dyshidrotic eczema are as follows:
- Stress. The condition tends to occur more frequently when you are under physical or emotional stress.
- Exposure to some metals. Getting in contact with certain metals such as nickel and cobalt increases your risk of getting dyshidrotic eczema-especially if you are working in industry.
- Sensitive skin. If you have a tendency of developing a rash after coming in contact with various irritants, then you are more prone to get dyshidrotic eczema.
- Atopic dermatitis. The condition may occur in some people who have atopic dermatitis.
4. Hand eczema
Eczema, which affects only the hands of a person, is referred to as hand eczema. You are more prone to have this form of eczema if your job requires you to regularly or frequently use chemicals that can cause irritation of your skin.
In hand eczema there is dryness, itchiness, and redness of your hands and they may also form blisters or cracks.

Causes of hand eczema
The trigger of hand eczema is regular exposure to irritating chemicals. Individuals who are prone to have this form of eczema are those whose jobs expose their hands to irritating chemicals. Such jobs are:
- Cleaning
- Healthcare
- Hairdressing
- Dry cleaning or laundry
Risk factors of hand eczema
Since the trigger of hand eczema is exposure to irritating chemicals, hence, certain jobs that expose you to these irritants make you more prone to get the condition. Therefore, the risk factors of hand eczema are the same as contact dermatitis. Furthermore, women are two times more likely to get hand eczema than men.
5. Neurodermatitis
Neurodermatitis is a condition of the skin that begins with a patch on your skin that is itchy and scratching it worsens the itching. Due to this cycle of itch-scratch, the affected area of the skin becomes leathery and thick. You can develop several such spots on your body specifically on your neck, wrists, legs, anal region or forearms.
Neurodermatitis also referred to as lichen simplex chronicus is generally a chronic condition; however, it is not contagious or life-threatening disease. But it can cause recurrent and intense itching and disrupt your quality of life quality, sleep, and sexual function.
Symptoms and signs of neurodermatitis
- An itchy patch or several patches of skin
- The scaly or leathery texture of the affected skin area
- A rough, raised patch or several patches on the skin, which are darker or red in color than the remaining skin
Neurodermatitis usually involves areas, which you can reach easily for scratching such as the neck, head, forearms, wrists, vulva, ankles, anus or scrotum. You can have intense itching that may be intermittent or persistent. You can scratch while sleeping and also as part of your habit.
Causes of neurodermatitis
What exactly causes neurodermatitis is not known. The persistent and recurrent scratching and rubbing that is associated with this condition may start with something, which simply irritates your skin including an insect bite or tight clothing. As you scratch or rub the affected area, the itching worsens. The itching increases the greater you scratch the area.
Risk factors of neurodermatitis
In certain cases, the condition is usually associated with other skin conditions (chronic) such as psoriasis, eczema, and dry skin. Anxiety and stress may also trigger itching.
The factors that make you more prone to get neurodermatitis are as follows:
- Your age and sex. Similar to hand eczema, females are more prone to get neurodermatitis than males. Furthermore, the condition occurs most commonly between the ages of 30 and 50 years.
- Other conditions of the skin. Neurodermatitis is more common in people who have a family or personal history of eczema, psoriasis, dermatitis or any other similar conditions of the skin.
- Anxiety disorders. Stress and anxiety may trigger the itching associated with neurodermatitis.
6. Nummular eczema
Nummular eczema is also referred to as discoid eczema or nummular dermatitis and is a type of chronic skin condition that results in the development of coin or disc-shaped spots on your skin. These eczematous spots are well-defined and usually quite itchy. A clear fluid may ooze from them or they may become crusty and dry.
Symptoms of nummular eczema
One of the most noticeable and common symptoms of nummular eczema is the occurrence of coin-shaped, round spots on your body. These lesions most often develop on your legs or arms, but they can also spread to the hands and torso. These lesions may be red, pink or brown in color. Some of them may burn and itch while others may leak fluid and form crust over them. The skin around these lesions can become scaly, inflamed or red.

Causes of nummular eczema
What exactly causes nummular eczema is unknown. But, many individuals suffering from the condition have a family or personal history of asthma, atopic dermatitis or allergies. Furthermore, individuals with nummular dermatitis also have sensitive skin, which is irritated easily. A reaction of the body to a bug bite or allergy to chemicals or metals may trigger the condition.
Some of the factors that may lead to the occurrence of nummular dermatitis are:
- Stress
- Changes in temperature
- Dry skin
- Undergoing surgery
- Environmental irritants including formaldehyde, soap, and metals
Risk factors of nummular eczema
The factors that make you more prone to get nummular eczema are as follows:
- Residing in a dry, cold climate
- Having dry skin
- Having a poor flow of blood or swelling in your legs
- Having any other form of eczema
- Undergoing surgery
- Having an injury to the skin, including an abrasion or insect bite
- Having a skin infection (bacterial)
- Some medicines
7. Stasis dermatitis
Stasis dermatitis is characterized by inflammation of the skin that develops due to poor circulation. It usually develops in your lower legs as the blood has a tendency to collect there.
Symptoms and signs of stasis dermatitis
The symptoms and signs of stasis dermatitis are:
- Discoloration of the skin
- Scaling
- Itching
- Ulcer formation
You can also develop symptoms and signs of venous insufficiency. These are:
- Swelling of the legs
- Calf tenderness
- Calf pain
- Heaviness or a dull ache in the legs that worsens on standing
During the initial stage, the skin over the legs may appear thin and itch, but you should not scratch it. Due to scratching the skin can crack resulting in seeping of fluid. Gradually, these changes in the skin may become permanent. The skin may harden, thicken, or become dark brown and this is referred to as lipodermatosclerosis. The skin may also appear lumpy. During the final stage, the skin may break down with the formation of a sore or an ulcer. The ulcers due to stasis dermatitis generally develop on the inner side of the ankle.
Causes of stasis dermatitis
Poor circulation leads to stasis dermatitis, which occurs due to a chronic condition referred to as venous insufficiency. The veins in your legs have valves (one-way) that help in keeping the flow of blood toward the heart. If there is malfunctioning of these valves, as happens in venous insufficiency, then the blood collects or pools in the legs instead of being pushed toward the heart. The pooling of blood in the legs leads to stasis dermatitis.
Congestive heart failure and varicose veins may also cause stasis dermatitis and leg swelling.
The majority of the conditions, which result in stasis dermatitis generally, develop as you become older. But there are several other causes that may cause the condition irrespective of your age, such as:
- Deep vein thrombosis (DVT) in the leg
- Surgery (using a vein from the leg for bypass surgery)
- Injury (traumatic) to the lower legs
Risk factors of stasis dermatitis
Stasis dermatitis commonly affects people who have poor circulation. The condition is also common in adults who are greater than 50 years of age. Furthermore, women are more prone to get the condition than men.
A large number of medical conditions and diseases can make you more prone to develop stasis dermatitis; for instance:
- Venous insufficiency (in this condition the veins in your legs are not able to send blood from the legs to the heart)
- High blood pressure
- Varicose veins (in this condition the veins in the legs become enlarged and swollen and are visible beneath the skin)
- Kidney failure (in this condition your kidneys are not able to remove waste products and toxins from the blood)
- Congestive heart failure (in this condition, your heart is not able to pump blood through the body efficiently)
- Obesity
- Multiple pregnancies
- Injury to the lower limbs
- Deep vein thrombosis (DVT) in the leg (in this condition a blood clot forms in the vein of your leg)
Your lifestyle may also affect the risk of getting stasis dermatitis. The risk is increased in the following scenarios:
- If you are overweight or obese
- If you are sedentary or aren’t active or don’t exercise
- If you stand or sit for a long duration of time without moving
What are the complications of eczema?
Some of the common complications of eczema are:
- Hay fever and asthma. In some cases, eczema precedes these illnesses. More than 50 percent of young kids who have atopic dermatitis get asthma and hay fever by the age of 13 years.
- Skin infections. Your skin may break from repeated scratching leading to cracks and open sores that may ooze fluid. These make your skin more prone to getting infected from viruses, bacteria, and fungi, such as the herpes simplex virus.
- Sleep problems. You can have sleep problems and poor quality of sleep due to the constant itching and scratching associated with the condition. The itch due to neurodermatitis may affect your sexual function, sleep, and overall life quality.
- In people with dyshidrotic eczema, the pain and itching may limit their use of feet or hands.
- Persistent scratching due to eczema such as neurodermatitis may lead to skin infection, permanent scars or changes in the color of the skin.

Untreated symptoms of stasis dermatitis may result in the following complications in the long-term:
- Osteomyelitis (an infection of the bone)
- Chronic ulcers of the leg
- A skin infection (bacterial, such as cellulitis or abscesses)
- Permanent scarring
How is eczema diagnosed?
No laboratory tests are needed to diagnose atopic dermatitis/dyshidrotic eczema/nummular eczema/hand eczema. Your healthcare provider may likely diagnose the condition by doing an examination of the affected area of your skin and also reviewing your personal and family medical history. They may also do a patch test or other tests in an effort to rule out certain other diseases of the skin or identify conditions that may accompany your dermatitis.
For instance, they may test a scraping from the skin to identify a kind of fungus, which is the cause of athlete’s foot. They may also do a skin biopsy to test for other diseases.
Your healthcare provider may identify contact dermatitis and also find out its potential cause by discussing the symptoms and signs of the condition with you, asking specific questions to pinpoint the specific trigger substance, and also examining the skin to record the intensity and pattern of the rash. They may also recommend doing a patch test that determines if you have an allergy to something. The test is especially useful in cases in which the rash recurs quite often or the cause of the rash doesn’t seem apparent.

During a patch test, the doctor will apply a small quantity of potential irritants (allergens) to patches that have adhesive on one side and then these are applied to the skin of your back. You have to keep these patches on the skin for at least two or three days. Take care to keep the back dry during this time. The doctor will then check the reaction of your skin under the adhesive patches and find out whether you need further testing or not.
Your healthcare provider may identify neurodermatitis by doing an examination of the affected area of the skin by finding out if you are scratching and itching the particular area.
Your healthcare provider may make a diagnosis of stasis dermatitis by examining the skin of your legs closely. They may also recommend a venous Doppler ultrasound-a noninvasive type of test in which your doctor uses sound waves to find out the status of the flow of blood in the legs.
Treatment of eczema
Eczema is usually a chronic condition. You may have to try a number of treatments over several months or years to bring it under control. And even in the case, treatment is able to control the symptoms, they may flare again.
Diet to treat eczema
Before starting with using the change of diet to treat eczema, it is important to rule out food allergy-related eczema. If you suspect the eczema is due to food allergy, it is important that you consult a medical specialist (clinical immunologist/allergy specialist) and a dietitian trained in handling food allergies before undergoing an elimination diet. This is to avoid unnecessary removal of foods/food groups from the diet. With an improper elimination diet, and without the supervision of a dietitian, nutritional deficiencies may result.
An elimination diet refers to a diet plan involving the removal of food(s) or ingredient(s) suspected to cause allergies.
- When symptoms improve, the suspected food(s) or ingredient(s) can slowly be added back to the diet to see if an eczema flare results.
- If no improvement is seen after two weeks, then it can be said that the eczema flare is not related to food.
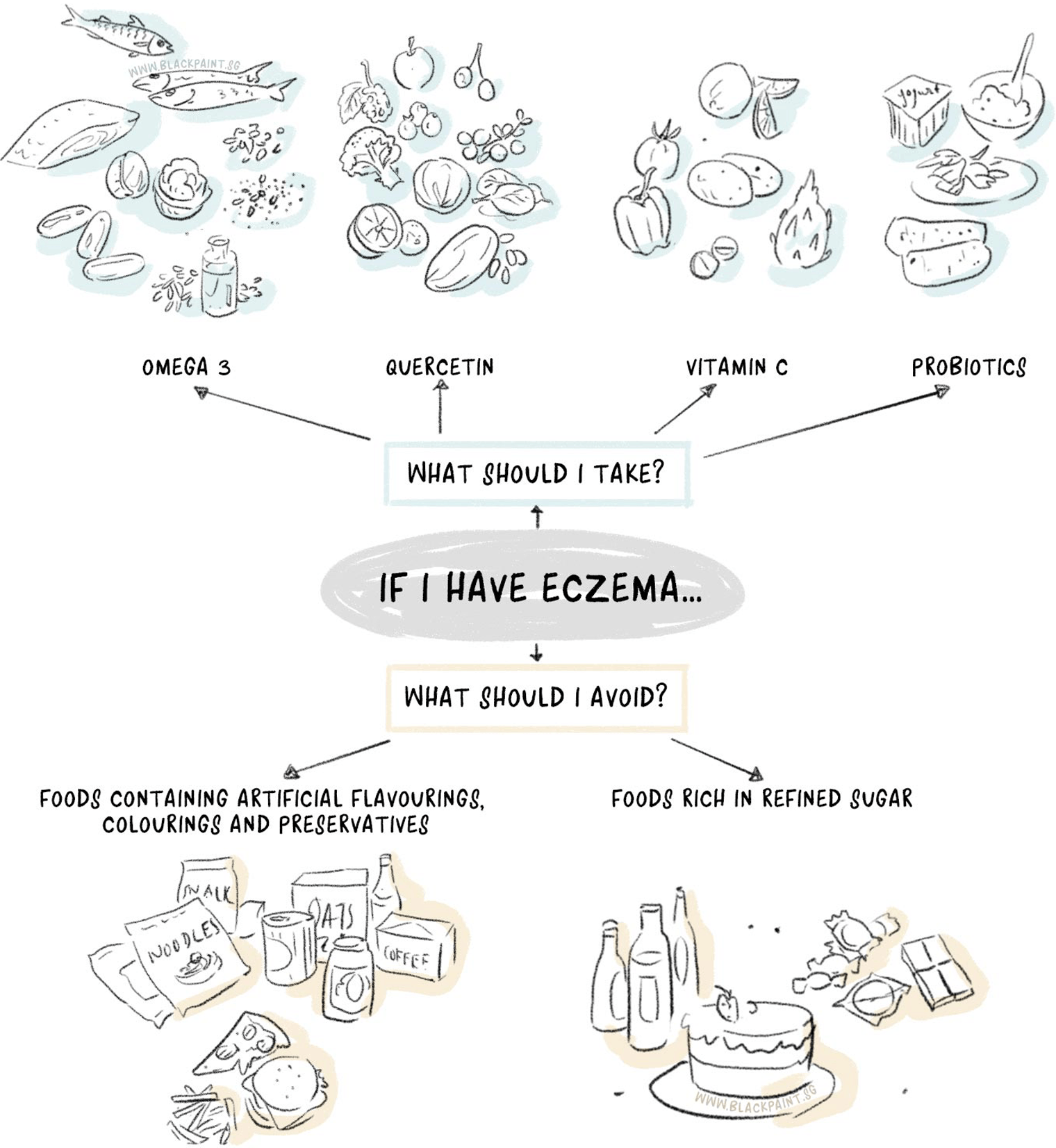
With food allergy-related eczema ruled out, below are what foods should be incorporated into the diet.
Foods rich in omega-3
Besides having cardiovascular benefits, omega-3 fatty acids can reduce the severity of eczema symptoms due to their anti-inflammatory properties. Omega-3 fatty acids are classified as essential fatty acids as our bodies cannot make them. The only way to get omega-3 into our bodies is through dietary means (i.e. from food). Examples of foods rich in omega-3 fatty acids are fatty fish (salmon, sardines, mackerel). For our vegetarian friends, the alternatives are walnuts, linseeds (or flaxseeds), and chia seeds.

Quercetin
Quercetin is a type of flavonoid (pigment) found in deeply-coloured fruits and vegetables. It displays antioxidant and antihistamine properties. As an antioxidant, its job is to “mop up” free radicals generated from oxidative stress. This slows down the aging process in our body. Oxidative stress generally arises from exposure to environmental/chemical toxins, leading stressful lifestyles, and eating a poor quality diet.
Sneezing, watery eyes, swollen eyes and/or lips, and red, itchy skin are common signs of an allergic reaction. This typically happens when the body comes into contact with a foreign substance. The immune system releases a chemical substance responsible for allergic reaction features (known as histamine) when it detects an allergy or sensitivity. Being a natural antihistamine, quercetin can help dampen the immune system’s release of histamine, thus lessening the allergic symptoms. In summary, quercetin is another anti-inflammatory food which you should add to your diet.
Good food sources of quercetin include:
- apples
- cherries
- dark-coloured berries (blueberries and blackberries) preferably
- cranberry
- green and black tea
- cruciferous vegetables (broccoli, Brussel sprouts)
- dark, green leafy vegetables like spinach and kale
- citrus fruits
- cocoa
- onions

Vitamin C
Vitamin C, known for its immune-strengthening and antioxidant properties, boosts your skin’s health. It helps build collagen in our skin and supports wound healing. Signs of vitamin C deficiency include scurvy (bleeding gums), easy bruising, poor wound healing, and the high tendency to fall sick.
As mentioned earlier, antioxidants help scavenge free radicals, which in excess can increase aging process in our bodies. One example would be reduced skin elasticity as free radicals would damage the collagen fibres in our skin. That is why it is unsurprising to find vitamin C added to topical products as well as oral supplements, e.g. collagen supplements.
Managing eczema with vitamin C
Eczema sufferers should incorporate more fresh fruits and vegetables into their diet. Here are some things to take note of:
- Vitamin C is a heat sensitive vitamin, so try to cook your vegetables in the quickest time possible. Compared to boiling (vegetables), steaming is the preferred option not only because it uses less oil, but also because it retains vitamin C better. Vitamin C is a water-soluble vitamin, and when we boil our vegetables, we usually end up throwing away the water, which means throwing away the precious vitamin C as well!
- Eat whole fruits and vegetables rather than juices, as juices contain little or no fibre. Fibre is important for bowel regularity and for good blood sugar control, thus keeping hunger pangs at bay and is also beneficial for people with diabetes.
Probiotics
Probiotics, as defined by the World Health Organisation, are ‘live microorganisms which when administered in adequate amounts confer a health benefit on the host’. As most of these probiotics are found in our gastrointestinal tract, oral consumption has been promoted to help achieve a healthy gut microflora. This helps in managing allergies such as eczema since eczema is an immune system response.
By incorporating probiotics into our diet, the immune system is strengthened indirectly as probiotics support a healthy gut lining. This is particularly useful in preventing leaky gut syndrome, a condition where the gut integrity is weak and damaged (i.e. “leaky”). A weakened gut integrity allows substances which it does not normally allow to pass through – such as proteins, toxins, undigested food particles – to enter the bloodstream. Our immune system senses these substances as foreign and goes into an (inflammatory) immune reaction. This immune reaction can trigger an eczema episode.

Probiotics and infants
There is some evidence that probiotics may help prevent an eczema episode in infants. A systematic review has found a decreased risk in eczema development (including atopic eczema) when probiotic supplementation is given to pregnant mums, breastfeeding mothers and infants. However, the authors of this review concluded there is insufficient evidence at this point to deduce with certainty that probiotic supplementation is an effective treatment for eczema. This is due to differences in study design and probiotic strains used in the studies reviewed. Other points to consider include dosage strength, the timing of administration and duration.
Probiotics in your diet
Whilst the jury is still out on whether probiotic supplementation can become the mainstream treatment of eczema, there is still some good in incorporating it into one’s diet. Including probiotic supplementation or probiotic-rich foods in the diet – since these friendly bacteria can assist in healthy digestion – helps reduce gas and bloating, and promotes bowel regularity. Fermented foods such as yoghurt, kefir, miso, kimchi, tempeh and sauerkraut are rich food sources of probiotics.
What not to eat?
If the type of eczema that you have is not related to food allergy, there are some ingredients in foods that can trigger or worsen the eczema symptoms. Examples are:
- Foods containing artificial flavourings, colourings and preservatives like fast food and processed foods.
- Foods rich in refined sugar – these foods are digested quickly, resulting in an insulin spike, and this is considered to be inflammatory for the body. Common examples include sugar-sweetened beverages, pastries, and cakes.
Medicines administered by heathcare professionals to treat eczema
Creams that help in controlling the itching and repairing the skin. Your healthcare provider may prescribe corticosteroid creams or ointments. You may have to apply this topical steroid one to two times per day for a duration of 2-4 weeks. You may apply cool compresses before rubbing the topical corticosteroids into the skin as it helps in getting the medicine more easily in the skin. Side effects may occur due to overusing these drugs such as thinning of the skin. Your doctor may also give you antihistamines such as Benadryl or an anti-itch cream (nonsteroidal) to control itching associated with the condition. Your healthcare provider may recommend topical medicated patches containing capsaicin 8% or lidocaine 5% for intense and persistent itching associated with neurodermatitis.
There are other creams that contain drugs referred to as calcineurin inhibitors including pimecrolimus (Elidel) and tacrolimus (Protopic), which your doctor may prescribe. These creams affect the immune system and are utilized by people who are older than 2 years of age to help in controlling the reaction of the skin. You must apply it according to the directions after moisturizing your skin. You should avoid going in strong sunlight after using these creams. An adverse effect of using these creams is that their use makes you more prone to develop skin infections.
Drugs to combat infection. If you are having a superimposed bacterial infection, then your healthcare provider may recommend an antibiotic ointment or cream. They may also recommend a short course of oral antibiotics to treat the infection. They may also recommend antifungal and antiviral medicines to control the associated viral and fungal infections.
Oral medicines for controlling inflammation. For cases that are more severe, your healthcare provider may recommend oral corticosteroids including prednisone. You should not use these drugs for long periods of time as they have serious adverse effects. In cases of neurodermatitis, your healthcare provider may give corticosteroid injections directly in the affected area of the skin so that it can heal.

Newer option in cases of severe eczema. A novel, injectable monoclonal antibody (biologic) referred to as dupilumab has been recently approved by the FDA (Food and Drug Administration). It is utilized to treat individuals who have severe disease and if the disease has not shown a good response to other options of treatment. It is an expensive treatment.
Drugs to control anxiety. Since stress and anxiety may trigger neurodermatitis, drugs to control anxiety can help in preventing the itching associated with the condition. An oral medicine referred to as N-acetylcysteine has helped some individuals with scratching and picking disorders in a small research study and hence may help people suffering from neurodermatitis.
Therapies to treat eczema
Wet dressings. This is an intensive and effective treatment used for severe cases of eczema in which the affected region is wrapped with wet bandages and topical corticosteroids.
Light therapy. This is used for individuals who either have a recurrent flare-ups after treatment or don’t improve with topical therapy. In its simplest form phototherapy or light therapy involves exposing your skin to natural sunlight in controlled amounts. In other forms, artificial narrow-band ultraviolet B (UVB) and ultraviolet A (UVA) are used either with medicines or alone. Though light therapy is an effective form of therapy to treat eczema, you should not use it in the long term as it may cause harmful effects such as making you more prone to skin cancer and premature aging of the skin. Due to these reasons, it is not used commonly in young kids and not used in infants.

Counseling. If you are frustrated or embarrassed by your skin condition, then it may help to talk to a counselor or therapist. Talking to a counselor can also help in learning how your behaviors and emotions can prevent or fuel scratching and itching. If you scratch and rub your skin habitually then biofeedback, behavior modification and relaxation techniques may help you in fighting this habit.
Injections of Botulinum toxin. If you have severe dyshidrotic eczema/neurodermatitis then your doctor may recommend injections of Botulinum toxin. This may help in reducing the itching and clearing the lesions and rough patches of the skin.
Your healthcare provider may recommend surgery to correct painful varicose veins. You can also control the stasis dermatitis by treating and controlling conditions, which result in venous insufficiency including congestive heart failure and high blood pressure.
Lifestyle and home remedies
Try the following self-care and lifestyle measure to soothe inflammation of the skin and reduce itching due to eczema:
Apply a moisturizer
For a person with eczema, the skin barrier is weak and usually drier due to loss of moisture, hence it is important to keep the skin well moisturised. Other factors that can further dry the skin include excessive washing, exposure to cold or hot temperatures (i.e. winter temperatures, taking hot showers or visiting saunas), and using harsh soaps. A dry skin will usually prompt one to scratch, and the more one scratches, eczema worsens. This “ itch and scratch” cycle is also distressing for the sufferer. Hence keeping skin moisturised is the key, as it becomes a protective barrier for the skin.
What type of moisturizer is good for eczema?
Moisturizers generally fall into three categories – ointments, creams, and lotions; the difference between them is the oil-to-water ratio that they contain. Of the three, ointments and creams are the best for eczema skin as they have a higher oil concentration, hence are much better at moisturizing skin than lotions. The (oil) barrier is needed to keep skin moisturized but also prevent environmental irritants from entering the skin. The best time to apply moisturizers would be immediately after washing your hands or showering.
Skin barrier creams are useful when used in conjunction with moisturizers. Such creams usually contain lipids and ceramides that are found naturally in healthy skin barriers. These creams help keep moisture in the skin and prevent entry of irritants, whilst allowing the affected skin to heal and become resistant to eczema symptoms such as itch and dryness. Skin barrier creams are typically applied to the area that is affected by eczema or as directed by your dermatologist.
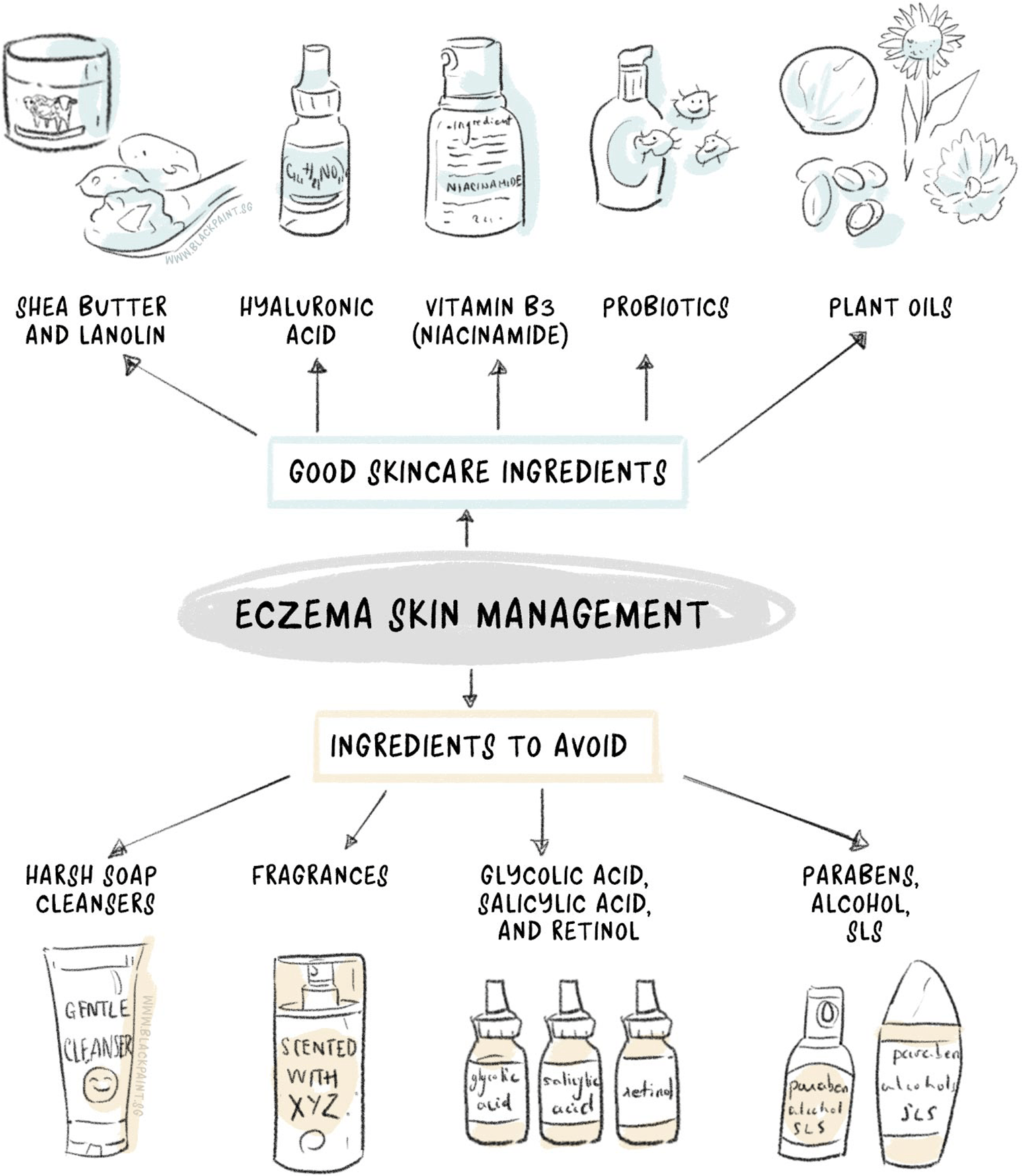
What to avoid in topical products?
- Soap cleansers
Some soaps can be harsh on your skin, and make it prone to eczema and dry out. Choose gentle soap cleansers or soap-free cleansers instead. - Fragrances
These may make your products smell wonderful, but did you know they can irritate the skin and trigger a flare? Choose products that say “fragrance-free” on the label the next time you shop for your skincare products. - Glycolic acid, salicylic acid, and retinol
These products are often not recommended for the eczema-prone skin as they tend to weaken its natural barrier. A weakened barrier means quicker moisture evaporation and increased vulnerability to environmental irritants. The end result is skin becomes dry and/or irritated, and an eczema results. - Parabens
One of the most common preservatives found in skincare products and cosmetics. They may keep skincare products and cosmetics “fresh” by preventing bacterial growth; but the downside is, parabens can irritate skin and cause eczema to flare up. Parabens can be easily identified from the ingredient list as they usually end off with “parabens”, e.g. methylparaben or butylparaben. - Alcohol
Alcohol-containing skincare products may give a cooling sensation (especially on a hot day!), but it is bad for your skin. Alcohol not only dries the skin, but it also weakens the skin’s natural (protective) barrier; resulting in a thin and irritated skin. Examples of the common alcohols found in skincare products include benzyl alcohol, denatured alcohol, isopropyl alcohol, ethanol, ethyl alcohol, methanol, and SD alcohol. - Sodium laureth sulfate (SLS)
A foaming ingredient commonly added to shampoos, cleansers, bubble baths and shower creams, to give you the “clean” feeling. Think of SLS as a detergent – that doesn’t sound nice, does it? Using SLS-containing skincare products may strip the layer of oil found naturally on the skin. This leads to dry, irritated, flaky and/or reddening skin.
Avoid the allergen or irritant. You must identify the cause of your condition (allergen/trigger) and avoid it. You may ask your healthcare provider to provide you a list of those products that contain the ingredient that causes the allergic reaction in you. Also ask about the products, which don’t contain the said allergen. In case you develop allergy due to a metal present in a jewelry piece, you can put a barrier between the metal and you and then wear it. For instance, put a piece of tape inside a bracelet or apply a layer of clear nail polish. Some of the triggers that you may avoid include harsh soaps, dryer sheets, fabric softener, household chemicals and cleaners, and getting cuts, abrasions, and scrapes on your skin. Some of the other common triggers of the condition are sweat, obesity, stress, detergents, pollen, and dust. Eczema flares may occur in children and infants from ingesting certain foods such as milk, wheat, soy, and eggs. To prevent dyshidrotic eczema, avoid exposure to salts of metals such as nickel and cobalt. Furthermore, after coming into contact with an allergen wash and rinse your skin thoroughly with warm water and fragrance-free, mild soap.
Don’t scratch the affected area. Instead of scratching when there is itching, try pressing the skin. Cover the affected area if you are not able to control the habit of scratching. For children, you should trim and cut their nails and make them wear cotton gloves while sleeping. You should also trim your nails, particularly if you have a habit of scratching during sleep.
Apply bandages. You can cover the affected area of the skin with dressings or bandages as it helps in protecting the skin and preventing scratching. These are particularly useful in case you have a habit of scratching while sleeping.
Apply wet, cool compresses. Moisten or wet soft and gentle washcloths and then place them on the rash for a duration of about 15 minutes to a half-hour to calm and soothe your skin. Repeat the process several times per day.
Soak in a lukewarm bath. Sprinkle some baking soda, colloidal oatmeal (oatmeal that is finely ground and is made especially for the bathtub such as Aveeno) or uncooked oatmeal in your bathwater. Soak in it for about 10 to 16 minutes and then pat yourself dry. Apply a moisturizer to your skin while it is still damp (within three minutes of taking bath as it locks in moisture). Limit your bathing time to about 10-16 minutes and also reduce the frequency of bathing. Use warm water and not hot water for bathing. Use gentle, mild soaps as antibacterial and deodorant soaps can cause dryness of the skin by removing natural oils. After bathing pat dry your skin gently and don’t rub your skin.

Protect the hands. Rinse your hands thoroughly and then pat them dry gently after cleaning and washing. Apply moisturizers multiple times all through the day. You may use gloves to protect your hands from exposing them to irritating chemicals.
Install a humidifier in your home. Dry, hot indoor air of your home can worsen flaking and itching and parch already dry and sensitive skin. You can use a portable humidifier in your home or attach one to your furnace to add moisture to your home air.
Choose gentle and mild soaps that don’t contain perfumes or dyes. Use soaps that are nonalkaline and superfatted. Make sure to rinse the soap off completely with water. Similalry, use mild and fragrance-free cleansers, detergents, makeup, and cosmetic products.
Wear smooth-textured and cool clothing. You can reduce irritation of your skin by avoiding clothes that are tight, scratchy or rough. Try to wear cool and smooth-textured clothes such as that are made of cotton. Moreover, wearing appropriate clothing during exercise and in hot weather helps in preventing excessive sweating.
Treat anxiety and stress. Stress, anxiety and other types of emotional disorders may deteriorate the symptoms of eczema. Hence, acknowledging these and improving the emotional health by using stress management techniques may help significantly in controlling the symptoms.
Take care when around pets. Irritants or allergens coming from plants; for instance, poison ivy may stick to pets and then spread causing allergic reactions in people.
Avoid activities that cause sweating and that produce rapid or quick changes in body temperature.
To help in the treatment of stasis dermatitis there are certain other things that you may do at your home. These include:
- Avoid sitting and standing for a long duration of time
- Propping up the feet while sitting
- Wearing compression stockings
- Wearing loose-fitting clothes to avoid irritation of your skin
- Avoid products containing lanolin, calamine or other lotions as they may dry the skin, topical antibiotic creams including neomycin as they may cause allergic reactions, and benzocaine and other medicines that numb the skin
- You can reduce the risk of getting stasis dermatitis by exercising regularly as it helps in improving circulation in your legs and reducing body fat. Also, limit the quantity of sodium in your diet to manage high blood pressure.
Natural Ingredients to treat eczema
Apart from the conventional treatments and lifestyle remedies, there are several natural ingredients that you can use to relieve symptoms of eczema. Some of these are:
Borage Oil
Borage oil is a rich source of GLA (gamma-linoleic acid), which is a kind of fatty acid that the body converts to PGE1 (prostaglandin E1). PEG1 acts similar to a hormone in the body and helps in decreasing inflammation associated with eczema.
A review of studies published in the ‘International Journal of Molecular Science,’ it was found that topical application of borage oil along with other essential oils that contain GLA has both anti-inflammatory and antioxidant effects and it helps in relieving symptoms of atopic dermatitis.
In another study published in ‘The Journal of Dermatology,’ it was found that children suffering from mild atopic dermatitis who wore undershirts having a coating of diluted borage oil had significant improvement in their symptoms of itching and erythema.
Borage oil is present in many of BLACK PAINT products including oil-water rose, German blue, and black paint soap.

Coconut oil
Coconut oil is another natural remedy that you use safely to relieve symptoms of eczema. About 50 percent of the fat in coconut oil is present in the form of lauric acid, which is a type of healthy saturated fatty acid.
An abstract published in the ‘Journal of the American Oil Chemists’s Society,’ states that lauric acid possesses antimicrobial properties; hence, it is quite capable of reducing viruses, bacteria, and fungi. This eliminates the risk of skin infection that occurs due to scratching and rubbing itchy skin.
Due to the presence of lauric acid, coconut oil also becomes highly absorbable; thereby, its skin moisturizing benefits are increased.
A 2014 study published in the ‘International Journal of Dermatology,’ stated that virgin coconut oil when applied topically to children suffering from mild to moderate atopic dermatitis was superior to mineral oil. This is because virgin coconut oil helps in improving the hydration of the skin.
Due to the anti-inflammatory properties of coconut oil, it may help in reducing the discomfort and inflammation linked to eczema. A study published in the ‘Journal of Clinical and Diagnostic Research,’ it was found that antioxidants are proved beneficial in relieving atopic dermatitis. Virgin coconut oil has antioxidant properties, due to which you can use it as an effective remedy to relieve the symptoms of atopic dermatitis.
Choose organic coconut oil of high quality that is either virgin or cold-pressed. This is to make sure that the oil that you apply to your skin is extracted without using any chemicals that may irritate the skin.
Coconut oil is present in several of BLACK PAINT products including black paint soap, sencha tea soap, matcha tea soap, houjisencha tea soap, koicha tea soap, and chamomile soap.
Jojoba oil
Jojoba oil is another effective natural remedy, which you can use to relieve symptoms of eczema. Jojoba oil forms a protective barrier on your skin and prevents the loss of moisture from it. This helps in preventing the occurrence of bacterial infections. Furthermore, it also has antifungal and antimicrobial properties due to which it helps in killing certain fungi and bacteria. This may help in reducing the risk of skin infection that can occur due to scratching the itchy skin in people suffering from eczema. Jojoba oil also has healing and anti-inflammatory properties; hence, applying it topically helps in relieving the symptoms of flaking, itching, and dryness associated with eczema.

According to a 2018 article published in the ‘International Journal of Molecular Sciences,’ jojoba oil contains a high amount of wax esters due to which it is a good repair agent for dermatoses such as atopic dermatitis and other types of eczema.
Jojoba oil is present in many of BLACKPAINT products including black paint soap, white paint soap, chamomile soap, koicha tea soap, houjisencha tea soap, matcha tea soap, sencha tea soap, best water, German blue, oil-water rose, argan balm, water cream, and esthe powder.
References
References
https://www.medicalnewstoday.com/articles/14417.php
https://www.mayoclinic.org/diseases-conditions/contact-dermatitis/symptoms-causes/syc-20352742
https://www.mayoclinic.org/diseases-conditions/dyshidrosis/symptoms-causes/syc-20352342
https://www.mayoclinic.org/diseases-conditions/neurodermatitis/symptoms-causes/syc-20375634
https://www.healthline.com/health/skin/nummular-eczema#causes
https://www.medscape.com/viewarticle/814683
https://www.healthline.com/health/stasis-dermatitis-and-ulcers#complications
https://www.mayoclinic.org/diseases-conditions/neurodermatitis/diagnosis-treatment/drc-20375639
https://www.mayoclinic.org/diseases-conditions/dyshidrosis/diagnosis-treatment/drc-20352348
https://www.mayoclinic.org/diseases-conditions/contact-dermatitis/diagnosis-treatment/drc-20352748
https://www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/diagnosis-treatment/drc-20353279
https://www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/symptoms-causes/syc-20353273
https://www.healthline.com/health/types-of-eczema#pictures
https://www.healthline.com/health/borage-oil#side-effects
https://www.mdpi.com/1422-0067/19/1/70/htm
https://www.ncbi.nlm.nih.gov/pubmed/20579590
https://www.healthline.com/health/coconut-oil-for-eczema#how-to-use-coconut-oil-for-eczema
https://www.ncbi.nlm.nih.gov/pubmed/24320105
https://aocs.onlinelibrary.wiley.com/doi/abs/10.1007/s11746-014-2562-7
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3919411/
https://www.medicalnewstoday.com/articles/323154.php
https://www.medicalnewstoday.com/articles/263027.php
https://www.healthline.com/health/evening-primrose-oil-for-eczema#uses
http://www.ijdvl.com/article.asp?issn=0378-6323;year=2008;volume=74;issue=5;spage=447;epage=452;aulast=Senapati
https://www.ncbi.nlm.nih.gov/pubmed/18078406
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5796020/
https://www.healthline.com/health/beauty-skin-care/jojoba-oil-for-face#side-effects-and-risks
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/eczema-atopic-dermatitis
https://www.healthline.com/health/skin-disorders/eczema-diet
https://www.webmd.com/allergies/allergies-elimination-diet
https://www.webmd.com/skin-problems-and-treatments/eczema/treatment-16/eczema-diet
https://draxe.com/quercetin/
http://www.who.int/foodsafety/fs_management/en/probiotic_guidelines.pdf.
https://www.medicalnewstoday.com/articles/318946.php
https://nationaleczema.org/eczema/treatment/
https://nationaleczema.org/eczema/treatment/moisturizing/
https://www.webmd.com/skin-problems-and-treatments/eczema/treatment-16/cosmetics-eczema-makeup
https://www.webmd.com/digestive-disorders/what-are-probiotics#1
https://www.healthline.com/nutrition/probiotics-101
https://www.aad.org/media/news-releases/could-probiotics-be-the-next-big-thing-in-acne-and-rosacea-treatments
https://www.simplyrecipes.com/recipes/waldorf_salad/
http://www.myrecipes.com/recipe/glazed-salmon-rice-bowl








